How does diabetes affect the eye? Diabetes is a leading cause of vision loss. Over time diabetes damages the blood vessels in the eye and can cause a variety of problems which the patient may not know until advanced stages.
The retina is the thin layer covering the inside of the eye. It is the most important part of the eye that allows you to see. When blood vessels are damaged in the retina from diabetes, several problems can occur.
The damaged blood vessels can leak fluid and cause swelling. This will cause blurred vision, and if left too long, can become permanent.
Also, over time the blood vessels can close off. With poor blood flow, vision will decrease and then damaging scar tissue can grow in the retina. This can lead to a retinal detachment and total blindness.
What are the symptoms of diabetes damage in the eye? Unfortunately there may not be symptoms until advanced, permanent damage has occurred. Blurred vision, large numbers of floaters or dark spots in the vision, and dimming of vision can occur.
How is diabetic retinopathy, or damage to the retina, treated? The most important treatment is careful control of the diabetes itself. Good blood sugar control and blood pressure management are essential to improving diabetic retinopathy. In earlier stages of the disease this alone can stabilize or even reverse the damage. In more advanced stages laser surgeries can be used for leaking blood vessels, and several medications are available for injection.
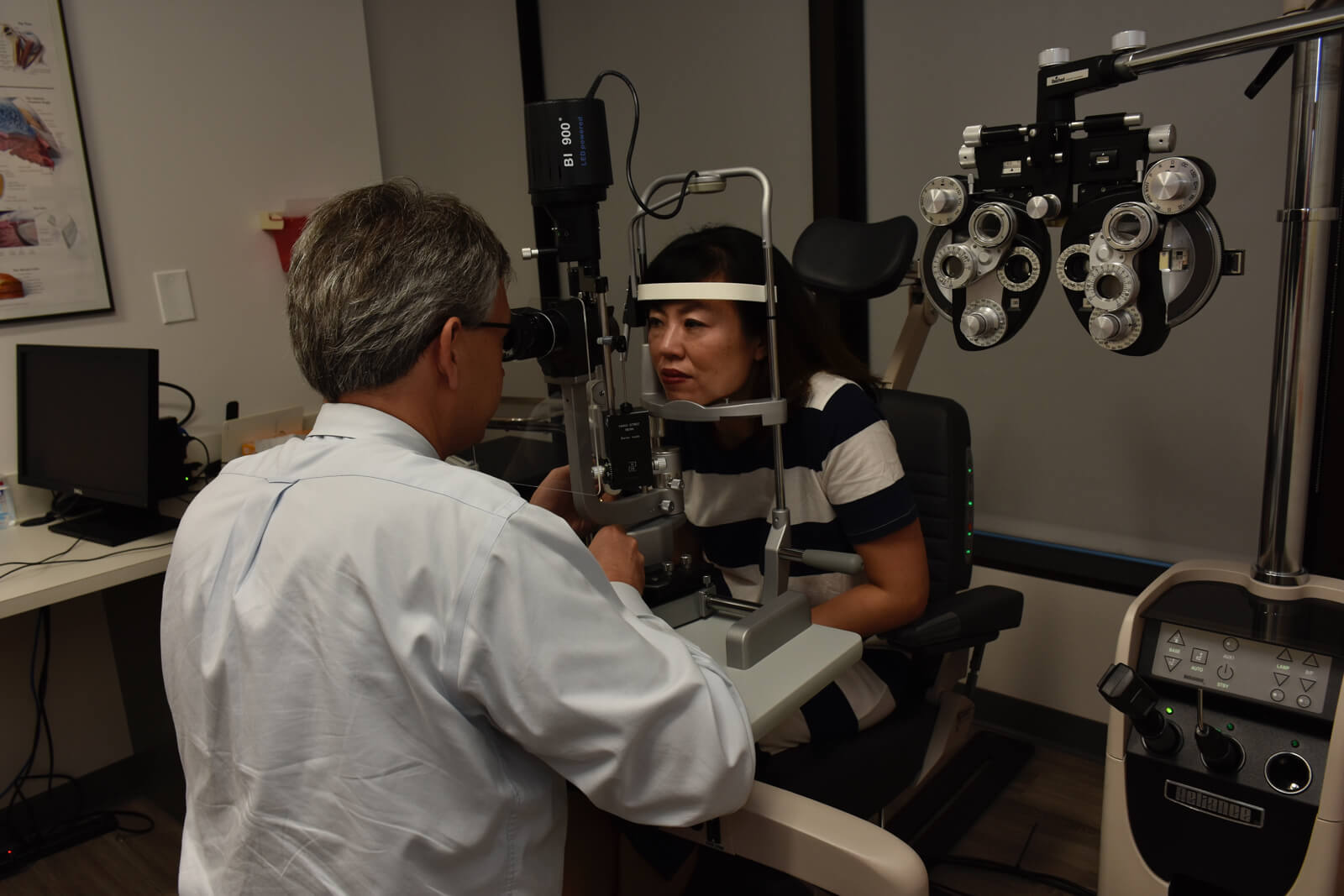
How often should a diabetic have an eye exam? Diabetics should be examined at least once a year and more frequently with more advanced retinopathy.
While diabetes certainly has the potential to cause blindness, careful blood sugar control and regular monitoring by your ophthalmologist can prevent vision loss.